How to improve the patient experience in your emergency department


Krista Burslam is a qualified Nurse who has worked extensively in Emergency Medicine in the UK and internationally. Before joining eConsult Health as the Clinical Director for Urgent and Emergency Care she worked as the Modern Matron at King’s College Hospital, Denmark Hill.
Emergency departments (EDs) are typically crowded and busy places, meaning patients are often frustrated and perhaps angry about how long they have waited. The wait can feel never-ending. The worry and anxiety keep building the longer you wait.
Often, by the time the patient has waited to even see a clinician they are grumpy. By the time they have waited a few hours, depending on how serious their symptoms are, the anger might have built up. The Urgent and Emergency Care Survey of 2018 reported that around 1 in 10 respondents felt threatened by other patients or visitors while they were in an ED.
Managing the patient experience is becoming an increasing part of the role of ED Matrons and staff across our urgent and emergency care departments. In 2011, The Design Council worked with several NHS trusts to produce its guide on ‘Reducing Violence and Aggression in A&Es’. One such hospital was St George’s ED in Tooting, where I was working as a Practice Educator and Senior Sister at the time.
We followed the Design Council’s guidance to redesign the waiting room at Queen Mary’s Hospital, Sidcup, ahead of launching the pilot for our digital check-in and automated triage software, eTriage, in late 2017. As eTriage has rolled out across other sites, we’ve learned even more about the impact digital check-in and triage has on the patient experience.
What’s the problem now?
When a patient arrives, they usually face a queue to speak to a receptionist or streaming nurse who will take their details and a few words about why they are there. If the patient is embarrassed about their symptoms, there’s often little to no privacy when they are in a queue and trying to talk to a receptionist behind a desk, barrier or a screen (even though the Design Council recommends removing glass screens).
Once the patient has been checked in, they sit. They wait. Their condition might be deteriorating, but it can be hard to know that, especially if they physically look alright. They will also likely be sat among other patients in an often crowded waiting room. Waiting rooms aren’t traditionally areas that allow for social distancing, which is a particular problem with COVID-19.
They will wait until their name is called, sit down with a streaming or triage nurse and tell them again about why they are here. The triage nurse will ask questions to assess the patient before, in most cases, they go back to the waiting room to sit and wait again. After a few hours, their name will be called, and someone will see them.
From the patient’s perspective, there’s are several areas of understandable frustration with the current process:
- Lack of privacy and dignity – when you might be feeling very ill, you’re still made to queue, to wait for hours, to be around others, and to repeat yourself to different people.
- Lack of space – waiting rooms are often crowded and as some of those people may have been there a long time, a natural tension can build up, especially when people are sitting in close proximity to other people.
- Uncertainty about what’s going on – you know you’ll be seen, but you don’t always know how long that will take.
- Not clear how patients are seen – sometimes patients who arrive after you are seen before you.
What impact can technology have?
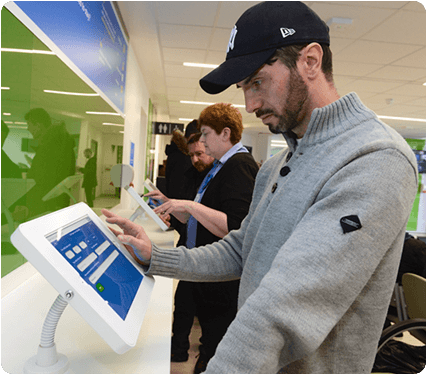
While an entire redesign for a department is often unfeasible, there are solutions that can be used within existing departments to help with the above issues. eTriage allows patients to check themselves into the department and provide their information in their own words and time. It ‘plugs into’ the reception area in the form of a bank of tablets that patients use as soon as they arrive.
Departments that have already implemented eTriage are noticing remarkable changes within their waiting rooms, with patient experience improving. Catherine Keegan, the ED Matron at Western Sussex Hospitals said that “without question, it has promoted privacy and dignity” for their patients.
Improving available patient information
eTriage allows patients to answer questions about their health and why they are at the department in their own words. It includes a mix of multiple-choice and free text questions to allow for structured information to be taken but also to allow for the expression of certain information in their own words.
“We wanted to find a better way to prioritise patients attending our emergency department, which is why we brought in eTriage. Patients now provide a documented record of their symptoms through a tablet at the front of the department which they can complete themselves. This means we get an understanding of their own perception of their condition, such as how much pain they are in, and of how urgent their needs are.”
Colin Dewar, A&E Consultant, Worthing Hospital
The self-service check-in process introduced by eTriage has also reduced the number of comprehension errors between patients and receptionists, as patients are inputting their own details into the system. Patients who don’t feel confident doing this can be supported by a family member. Otherwise, they can be helped by a receptionist, who is now free to be on the waiting room floor and can ensure infection control and social distancing measures are in place.
By collecting patient’s information as soon as they walk through the door you and your staff know about them and their symptoms as quickly as is physically possible. Hospital departments that have started doing this are now collecting patient information, including Emergency Care Data Set (ECDS) questions, directly from patients within 5 minutes of arrival.
“Patients like the fact they are in control – patients want to tell you things in their own words. Our patients are satisfied that they have been able to provide their information, that the department has that knowledge about them, that it’s all logged and taken into account.”
Catherine Keegan, ED Matron, Worthing Hospital
It’s also flexible and easy to update eTriage as and when guidance changes. During COVID-19, questions were added overnight as guidance changed, for example with the Danish mink variant, meaning that nurses didn’t have to worry about ensuring they asked these new questions to patients. It also meant that staff were collecting information about patients and their symptoms as soon as they walked into the department, minimising the risk of spreading the virus if they displayed any symptoms or detailed worrying information.
Improving patient privacy
There’s no need for patients to queue to see a receptionist – banks of tablets now allow them to do this themselves, providing them with additional privacy. Some practices have added the tablets along a bank, with adequate spacing between each one, whilst others have created individual booths around each tablet.

By not having to voice the reasons for being at the department, patient privacy is increased. This is especially true in departments that may have limited space or be smaller than they would ideally be, based on their capacity or the number of patients that attend the department.
“Patient dignity and privacy is a key consideration – the eTriage tablets avoid people from having to divulge their condition or concern in front of others at reception. It feels very immediate, there’s lots of tablets for patients to interact with so no one has to wait now. As patients have interacted immediately, and they know they are ‘in the system’ it’s a much better experience for them. It means the waiting room is much calmer than before.”
Catherine Keegan, ED Matron, Worthing Hospital
Reducing waiting times
As part of this digital check-in process, the clinical questions that patients answer are being used behind the scenes to triage the patient, assigning them a priority score. This information is fed into the clinical system in an easy to read and structured way. Particularly important, it alerts clinicians to the sickest patients in their waiting room, so that they can be assessed first.
You can now quickly call out your highest priority patients. Using the structured information they have already provided, you or your triage nurse can validate this information with them, ask any additional questions and make a decision about next steps then and there. For example, they might need some pain relief or the nurse might need to arrange some investigations for them before they move on to the rest of their journey.
This streamlines the patient’s consultation – they only need to provide their information once, in detail, when they enter the department. As you know how sick they are, you can assess those patients that present the biggest risk first, validate the information provided through eTriage and decide what needs to happen next.
“eTriage provides multiple benefits for our patients by reducing waiting times, flagging life-threatening conditions more quickly and taking history on arrival to ensure the right care is given to those who need it first.”
George Findlay, Chief Medical Officer, Western Sussex Hospitals
Conversely, it also allows you to identify patients that could be best helped in another healthcare setting, such as at their GP practice or within the community. These patients would previously have been likely to wait for several hours, but now you can identify them quickly, verify their information and let them know where to get the best care for their needs.
This technology doesn’t remove the human touch, or the need for trained and experienced nurses or receptionists. It can, however, create efficiencies within departments and improve the processes and transfer of information between patients, clinicians and clinical systems. Ultimately, the goal is to achieve a better working environment for department staff as well as patients, which is what eTriage customers are already experiencing.