Western Sussex Emergency Department Performance Evaluation
Executive Summary
Western Sussex Hospitals wanted to future proof their model of care, using technology as an enabler to prioritise sick patients turning up to their Emergency Departments and improve patient flow to reduce times to treatment by clinical decision makers. They believed that eTriage, a digital triage solution for Urgent and Emergency Departments that automatically checks in and triages patients by clinical need to ensure they get the right care quickly and safely, would aid with this.
In order for eConsult to successfully implement eTriage within Western Sussex Hospitals (St. Richards & Worthing) both parties decided to work to a highly detailed and specific timeline and execution process.
This joint approach built trust between eConsult and Western Sussex Hospital Trust and allowed for productive collaboration between the project teams.
Results over the case study period showed reduced waiting times, a reduction in time to treatment, an improvement in the percentage of patients triaged within 15 minutes of arrival, and an improved flow through the Emergency Department.
What did we evaluate?
How does using the eTriage system affect waiting times for service users coming through the Emergency Department?
- Has the time from arrival to initial assessment decreased?
- Has the median time to treatment decreased?
- Does the implementation of eTriage result in faster movement through the hospital system?
- Has eTriage enabled quicker and safer risk stratification of patients presenting in the waiting room?
Do staff like using eTriage above current methods of triaging?
- What are the features of eTriage that are most liked?
- Is the system easy to use?
- Where can eConsult focus on to improve the user experience?
- Does eTriage support the staff in their decision making?
eTriage at St.Richards Hospital
Total daily submissions of eTriage
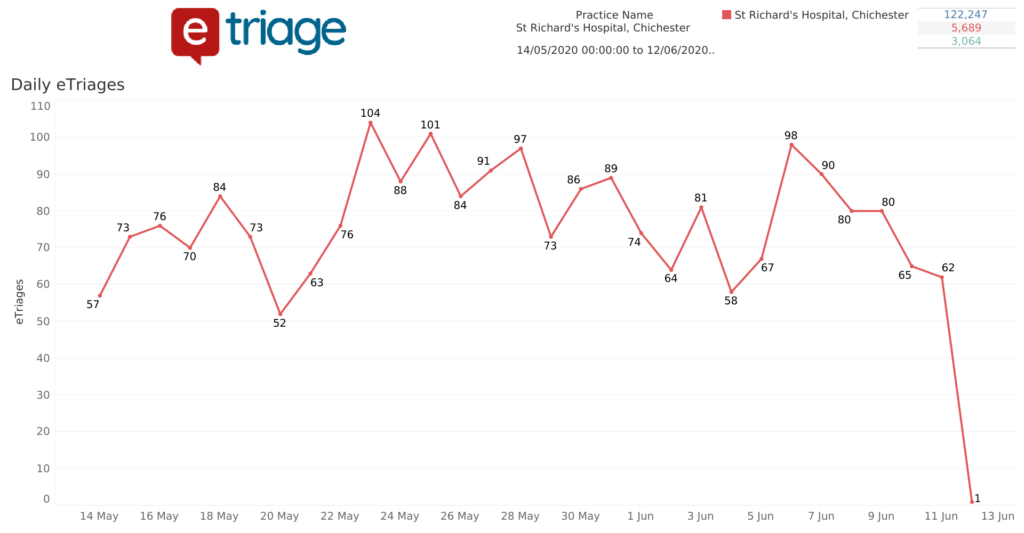
- St Richards has seen an increase in daily submissions since launch to a peak of 104 submissions per day in May
- Total eTriage submissions account for approximately 80% of total attendances
Monthly submissions of eTriage
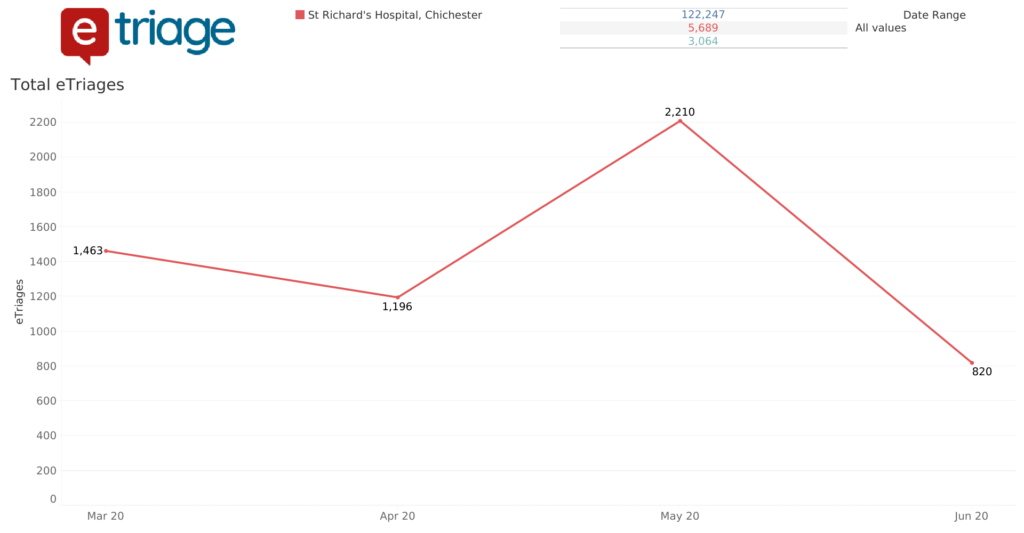
- The above details the total monthly eTriage submissions within St Richards, building in volume to a total of 2,210 eTriage submissions in May which is an increase of 1,014 from April
- The high proportion of attendance figures using eTriage suggest that the patients are able to use the system without issue
Time to Triage

- eConsult aims to decrease the time to triage to 15 minutes or less with the eTriage system.
- Since the implementation of eTriage at St Richards hospital there has been an increase in patients that are being triaged within 15 minutes or less.
- Time to assessment reduction would infer improved departmental patient flow.
- It should be noted that this time period coincides with the COVID-19 pandemic.
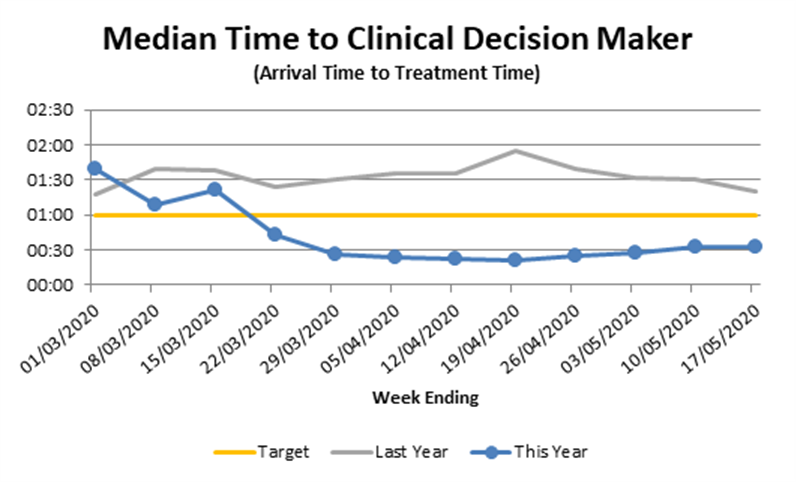
- St Richards Hospital has seen a decrease in the time to treatment post implementation.
- Patients are now being treated as quickly as 30 minutes post arrival in comparison with last year with patients being seen 90 mins post arrival.
- Reducing the time to treatment and the total wait time for patients indicates faster movement through the hospital system, which is a key improvement.
- It should be noted that this time period coincides with the COVID-19 pandemic.
Weekly P1-P5 figures
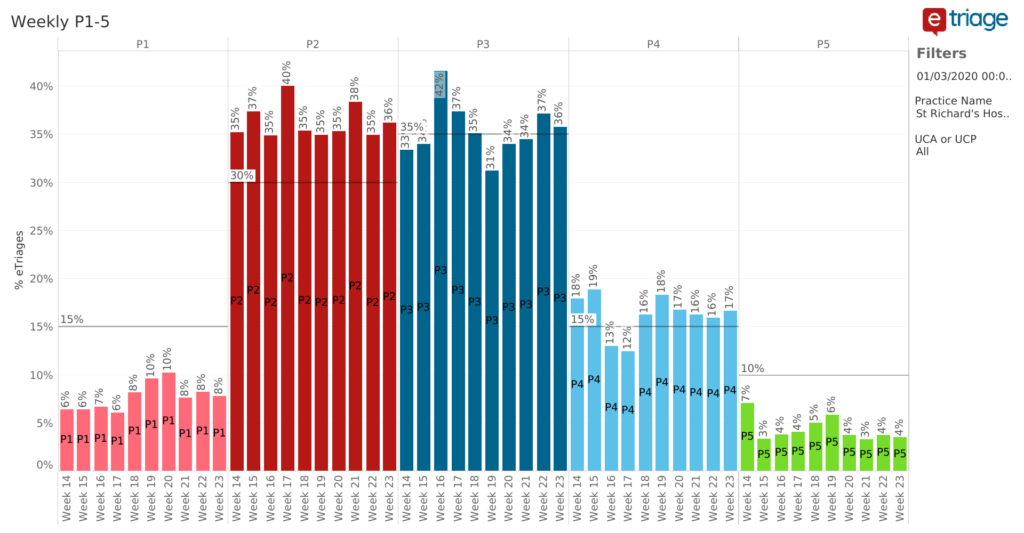
- This graph shows the percentage of P1-P5 ratings weekly (from March to June) categorised by eTriage following a completed submission.
- We can see that P2-P3 ratings are the most frequently used category rating for patients.
- These figures can coincide with the previous chart detailing time to treatment. Patients categorised as P2-P3 are seen by a clinician within 30 mins from arrival.
Summary Data
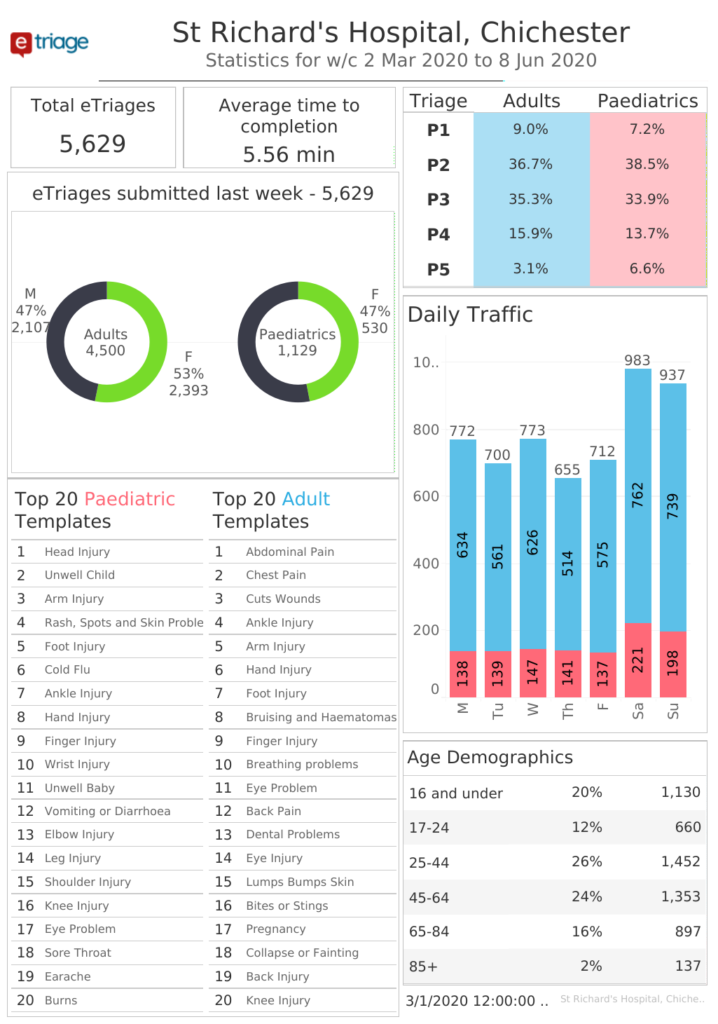
- This image provides a summary of eTriage usage within St Richards Hospital.
- We can conclude that the majority of hospital attendees are female adults aged between 25-44 with the top template being Abdominal Pain. 36.7% of Triages are categorised as P2 and the average time to completion is 5.56 minutes.
Staff feeback
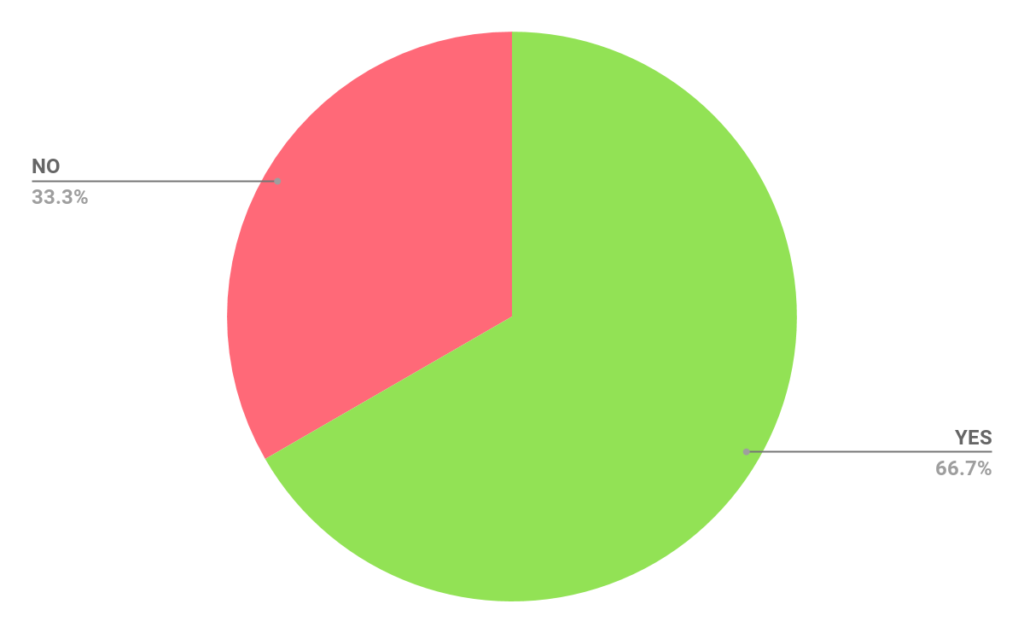
Has the flow of the department changed for the better since you have started using eTriage?
For Example: The flow of patient attendances and patient queuing
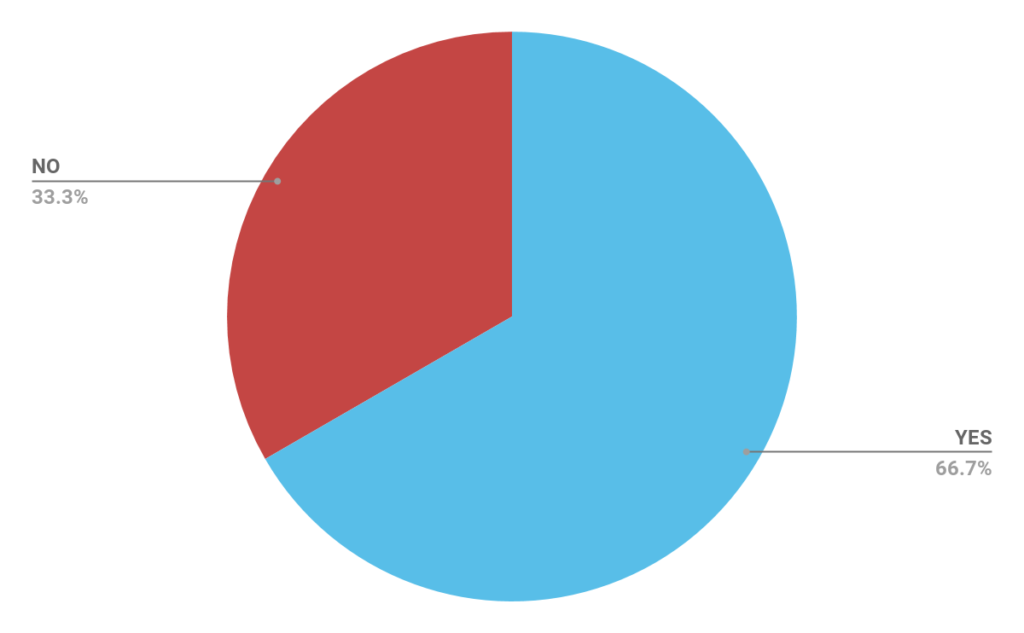
Has eTriage helped free up time for other tasks?
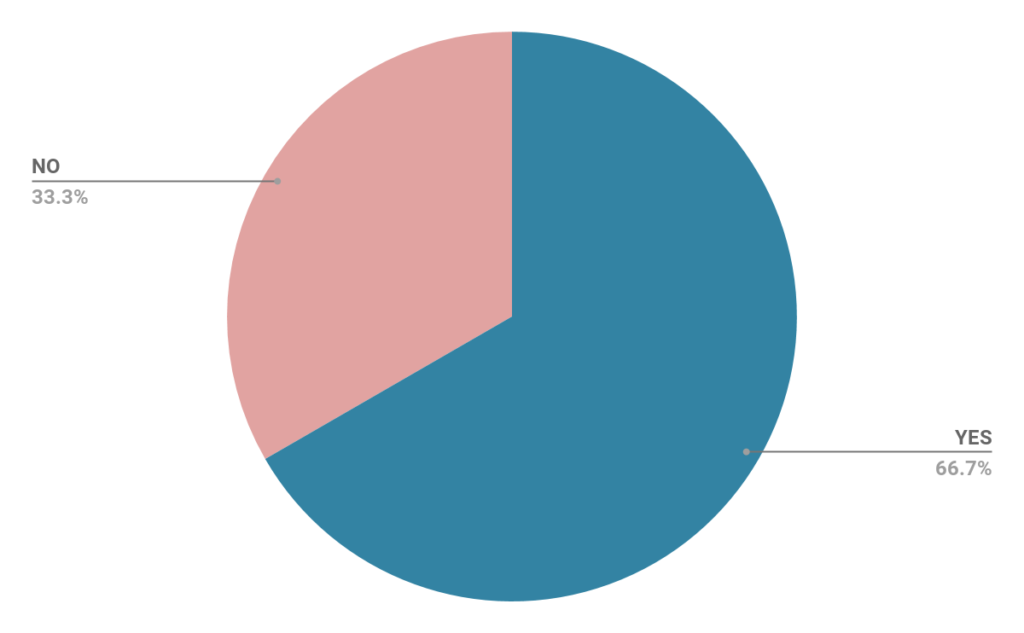
Did your team receive enough training from eConsult?
How would you rate the on-site support from the eConsult team during and after launch?
With regards to post installation support 100% of respondents believed that the support provided by eTriage prior and post implementation was very helpful.
Tell us what you found helpful about eConsults on-site support
- Lead Receptionist – “Able to troubleshoot issues straight away”.
- Care Group Manager – “Approachable, nothing was too much trouble”.
- Lead Receptionist – “Quick responses to emails”.
What was your biggest concern while eTriage was being implemented?
- Lead Receptionist – “Elderley/Vulnerable people being able to use eTriage”.
- Care Group Manager – “Timescales, Interoperability and estate management. Quality of estate finish”.
What other improvements has eTriage delivered?
- ED Matron – “Improved and highlighted the need to embrace the electronic innovations that are available to augment patient assessment, care and safety in the department, further reducing the risk in the waiting room from the ‘unknown’”.
- Practice Development Nurse – “Increased safety in the waiting room, it has enabled us to see who needs prioritising whilst they wait to be validated”.
- ED Matron – “ Without question promoted privacy and dignity for our patients!”.
- ED Consultant – “Freeing up of receptionist time, removal of lengthy queues at reception desk”.
- ED Consultant – “ Patient record of response”.
From the above it is clear the feature at which the clinicians enjoy about eTriage is the increase in patient safety, patients are seen based upon priorities, those that are prioritised highly (P1) are seen quickly.
Has the time to initial assessment improved since the implementation of eTriage? If so by how much?
- ED Matron – “It has been difficult to clearly identify progress consistently due to COVID affecting our ambition to achieve the majority of patients booking in by eTriage. however, those that have, stimulate a quicker response from the clinician to validate the assessment”.
- ED Matron – “eTriage has helped us to mitigate the patient safety risks associated with an overcrowded waiting room, by providing a robust clinical priority score”.
- ED Consultant – “Yes – enabled clinicians to see patients direct if available as initial parts of triage done”.
- Emergency Nurse Practitioner – “The P1 and P2 patients are assessed sooner than lower categories.”
- ED Consultant – “Some issues around over-triage. Record of patient response useful”.
Has there been an increase or decrease in overrides of booking priorities (P1-P5)?
- ED Matron – “Increase – mainly due to pain scoring and local policies for certain conditions”.
- ED Consultant – “Anecdotally patients tending to be downgraded at point of nurse triage, but higher eTriage category helping to flag up those injuries in significant pain, therefore, added quality benefit of reducing time till analgesia given”.
Do you have any clinical concerns about eTriage?
- ED Matron – “No”.
- Practice Development Nurse – “ Not clinically, we have found that patients’ perception of their pain often over triages them”.
- ED Matron – “No”.
- ED Consultant – “ No, and no clinical incidents have been brought to my attention when on shift either “.
- ED Consultant – “ Small amount of under triage needs to be investigated”.
How could the initial implementation of interoperability have been improved?
- Group Head of IT – “No detailed task by task project plan was produced at the initiation, led to lots of wrong assumptions being made, lack of clarity over exactly what was expected at various stages”.
- IT – “As a first for an implementation within an Acute Trust, apart from understanding how different we work compared to Primary Care, I don’t see how this could have been improved. Communication has worked well “
Can existing interoperability between eTriage and your clinical system be improved?
If so, tell us how.
- Group Head of IT – “ Yes. eTriage needs to be expanded to fully support ECDS data collection”.
- IT – “A test system (within SEMA) but this is something we are aware of and is not possible at this time “.
Did you receive enough support from the eConsult team during User Assessment Testing (UAT)?
- Group Head of IT – “Yes”.
- IT – “Yes”.
Could we improve the UAT Process in any way?
- Group Head of IT – “Full test environment required. (Test eTriage, Test spine, Test Trust system)”.
- IT – “No”.
How would you describe the teamwork between eConsult and Western Sussex during the implementation process?
- IT – “Very Good”.
What made the teamwork between eConsult and Western Sussex good?
- IT – “Very easy and always on hand to ask questions and resolve issues. Along with being flexible and understanding during implementation”.
Have you had enough support from eConsult during issue resolution?
- Group Head of IT – “Yes”.
- IT – “Yes”.
eConsult releases happen at 4 am every two weeks. Has this caused any issues?
If so tell us more
- Group Head of IT – “any downtime is a bad thing in Acute environments, where 24x7x365 is required.”
- IT – “Not that I am aware of. I don’t believe they have. We are always notified before these are due to happen”.
What can we change or add to make eTriage better?
- IT – “ Development will be key and it will be exciting to see this along with any other changes in the future”.
Our On-Going Story
Project Mangement
- Formalised check-ins – eConsult and Western Sussex have a scheduled bi-weekly post-implementation call to discuss the status of the system, any impromptu issues that they may be having and also to answer any questions that have arisen from usage.
- Formalised feedback process – eConsult have formulated a feedback form for staff to complete and detail how they feel about the implementation process, the overall eTriage system and its effectiveness within the department. They are also able to voice any concerns that they have about the system and also feedback any improvements that they believe would aid in the betterment of the department.
Governance of Product
- Performance Dashboard – eConsult have numerous live dashboards that we use to track the usage of eTriage across different sites. From these dashboards eConsult can observe the performance of eTriage post-implementation and draw quantitative data that can be used to better understand the implications of the system post-implementation.
- Auditing with the Clinical team – Based upon feedback received from users, eConsults internal clinical team meet weekly to determine what templates are beneficial, which templates need to be added to aid in better use of the system, and which need to be updated to keep in line with latest medical guidelines.
- Feeding into the Clinical Governance process – Patient safety is of paramount importance. The eConsult Clinical Governance team meets bi-weekly to create clinically-validated questions, and internal flagging processes that are reviewed and consistently updated to ensure that patient safety is at the forefront of eTriage.
eTriage is a digital triage solution for NHS Emergency Departments and Urgent Care Centres, developed by clinicians. eTriage was designed to automatically check-in and prioritise (triage) patients upon arrival to an emergency department. eTriage speeds up the streaming process, identifies sick patients earlier, reducing the waiting time and time to treatment within the department and delivering improved patient journeys.
Patients enter their own clinical history on tablets eTriage automatically books in and triages your patients by clinical need, ensuring your clinicians deliver the right care to the right cases.
eTriage has been designed by NHS clinicians and triages patients within 4 minutes of arrival. As patients provide their history and check-in at the same time, clinical staff are better informed of the patient’s condition as soon as they complete the eTriage form. Automatic triage into 5 priority categories (Manchester Triage), with alerts integrating into the clinical system, allows urgent patients to be flagged to clinical staff and attended to first.
