We can’t achieve remote consultation targets with video or telephone alone – we need both.
Outpatient care is a problem area primed and ready for innovation and service redesign.
There were 125 million outpatient appointments recorded in HES data in 2019-20, (67% more than ten years ago) but only 96 million attendances. Higher and higher volumes of appointments year on year mean that any breakdown through non-attendance is having a larger and larger overall economic and clinical effect as a whole.
The average outpatient appointment cost is approximately £120 and outpatient services currently account for approximately 7% of the NHS budget. Missed appointments were estimated in September 2018 to cost the NHS around £700 million.
Since the start of the COVID-19 pandemic in March 2020, there’s been a big rise in digital usage across the NHS, from online consultations in primary care to remote consultations in outpatient departments. In particular, the usage of video consultations has increased in secondary care in order to try to reduce the number of physical appointments across NHS Trusts and Foundation Trusts to avoid the spread of Coronavirus.
NHS England and Improvement procured and funded a provider for video consultations to enable access and uptake quickly. As part of the NHS Long Term Plan, there is also an aim for up to a third of the face to face appointments delivered in outpatient care to be avoided by 2024. It’s claimed this would save NHS England around £1.1 billion a year as well as saving patients 30 million visits to hospitals. In order to do this, the NHS is looking to embrace technology and arrange services around patients’ lives.
The NHS website says that remote consultations are ‘often more convenient for patients, saving them time and money and reducing the stress of travelling to their appointments… as well as being more environmentally friendly… [meaning] patients are less likely to cancel or not attend their appointments.’
We fully agree with this — but at the same time, we think there’s room for improvement, as is often the case with any system implemented during a crisis. We also spend a lot of time listening to clinicians and NHS colleagues and patients to understand what challenges they currently face and how we can support them to ease these annoyances.
That’s why in 2016 we created an easy to use web-based video consultation system, Q health. Our aim was to build a safe, secure and easy to use the platform to connect doctors and patients online, removing barriers to accessing care when it was needed, whilst keeping to the founding principles of the NHS. Since then, Q health has gone on to set precedents in video consulting nationwide across health and social care.
Challenges to widespread roll-out of remote consultations
There are challenges to this aim to deliver a third of outpatient appointments remotely. With less than 3 years to go to the target date, they need to be overcome or factored into decision making now. Whilst many are patient-related, there are others that commissioners and clinicians can tackle by making the right decisions now.
Digital skills and exclusion
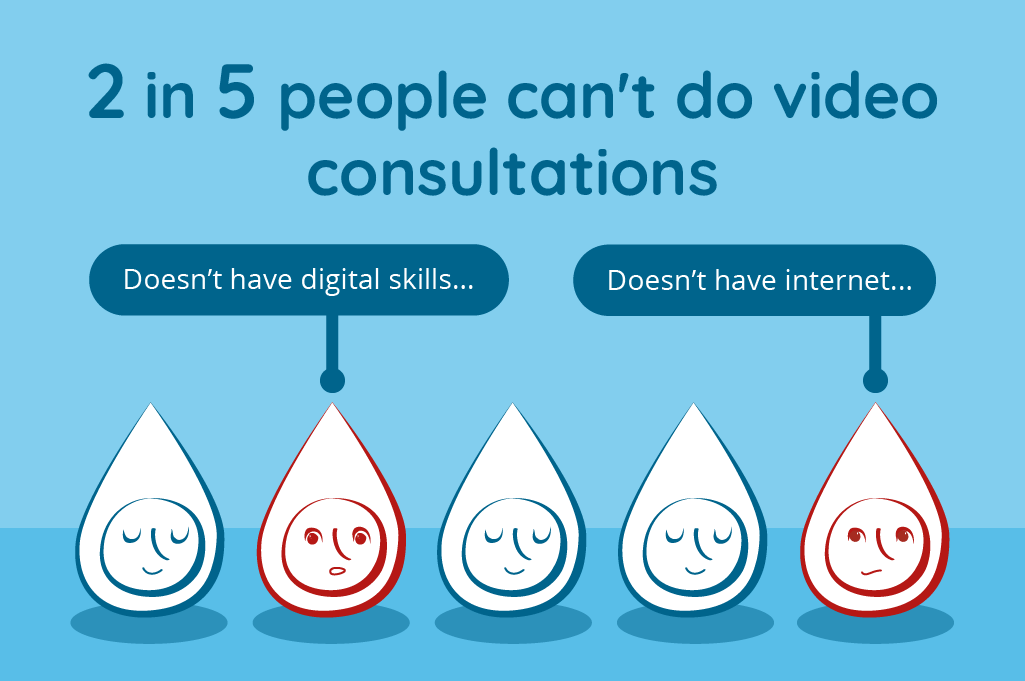
The 2019 Consumer Digital Index showed that 11.9 million people, or 22% of the population, do not have the digital skills needed for everyday life in the UK, with this expected to be 8% by 2030. Around 5 million people never go online at all. This means that many patients might not be able to benefit from video consultations with their clinician simply because they aren’t familiar with or aren’t able to access or use digital technology.
Whilst 90% of households have internet access, only around 78% of people go online using a mobile device. That means they might not be able to use smartphones in the manner needed to join a video consultation waiting room.
Both patients and clinicians need the flexibility to use the right tools for the right patient and at the right time. Patients might need support to try using new methods of communication, and an easy to use system can help to lower some of these barriers. However, many remote consultation providers at the moment do video or telephony – not both. This makes it more complicated for patients to get familiar with the technology they’ll be using to connect with their doctor.
Connectivity
Whilst superfast broadband is now available to over 95% of households, speeds vary across cities. Mobile connectivity is improving but the quality of coverage varies across networks and between as well as within cities. Coverage is also widely affected by events such as big football matches or by surrounding buildings.
Previous research in Wales into video consultations in outpatients departments showed that the most reported challenge by clinicians were technical issues associated to poor audio, visuals, internet or device (those who reported these issues happening ‘a lot’ ranged from 15.7% to 8.5%). This is often through no fault of the patient or the clinician, but simply a byproduct of infrastructure issues.
It has meant, however, that many specialist clinicians have not yet embraced video consultations. There are known benefits for the use of video consultations with patients, as they:
- Increase rapport with patients
- Improve clinical confidence
- Provide useful visual assessment opportunities
As a result, a lot of remote consultations have primarily been carried out over the telephone — most patients can easily pick up a telephone (mobile or landline) and every clinician can reliably make a call (again, mobile or often landline in outpatient departments). We know that due to the above issues of connectivity challenges and a lack of confidence or ability to connect, many clinicians are wasting a lot of their consultation time trying to actually just connect to their patients!

This means either trying and failing to connect via video and having to switch to telephone, or at worst having to reschedule appointments. Practice varies as to when clinicians record these as a ‘non-attendance’ but it’s clear that it wastes people’s precious time. It also doesn’t allow hospitals, as systems, to deliver the care activities that they are funded to provide.
Creating solutions that overcome challenges
These challenges have led us, as technologist clinicians, to think about how this ‘two tier’ system of video or telephone could be improved, for clinicians and patients alike. It makes sense to be able to tap into the benefits of video where it is possible to do so, whether for rapport or to provide a much needed visual aid, but then also to use the telephone where the circumstances require it.
When we went back to first principles, we found ourselves asking the question ‘Why would you not have a system that could transition between telephone and video, depending on the circumstances?’
When we try to cater for all we can enhance the sustainability of remote consultations. This means we can save patients a lot of hassle in no longer having to find a parking space and pay for the notorious NHS hospital parking prices, or pay for a bus or taxi. We can also try our best to protect their health and avoid them picking up a bug in the waiting room, whilst also doing our bit to protect the planet — 5% of all traffic is estimated to be generated by the NHS.
When remote consulting is done well, patients and clinicians love it. They just need the right tools in hand — or on their desktop. That’s why we’re offering all outpatient departments a free trial of our video and telephony consultation platform until 31st March 2022.
