How we analysed pain scores to reduce inappropriate redirection and improve the patient experience
After analysing 5,000 urgent warning redirections on an anonymised basis, we discovered that musculoskeletal (MSK) questionnaires made up around 19% of these urgent warnings. Further analysis found that 31% of these MSK urgent warnings were related to a question about the patient’s perception of their pain.
From numerical to functional pain questions
When patients report pain in their online consultation, we ask them to score it, often using a 10 point analogue rating. Initially, scores of 7 or above were urgently redirected. However, analysis of eConsult activity, along with feedback from our GP users, showed that patients’ subjective pain scores are not reliable indicators of how urgent a symptom is.

Our Clinical Team reviewed the pain scores and associated question sets. Out of the 31% of urgent warnings related to pain scores, 10% were deemed high-risk, such as those linked to chest or abdominal pain. Around 21% were deemed a lower risk, for example, those associated with joint or limb pain.
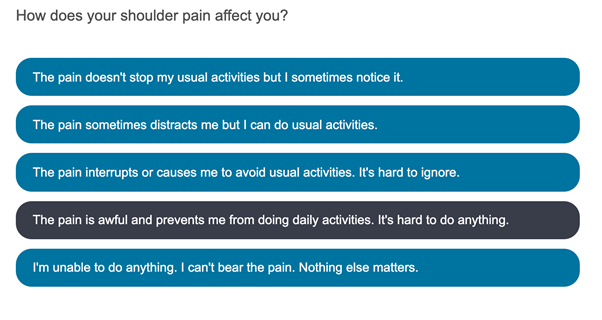
As a result of this, we updated ten of our MSK questionnaires to stop them from triggering an urgent redirection if the patient indicates a 7 or higher pain score. We have also added a functional pain score to these templates so that the clinician can understand the impact of the pain on the patient.
What impact has this change had?
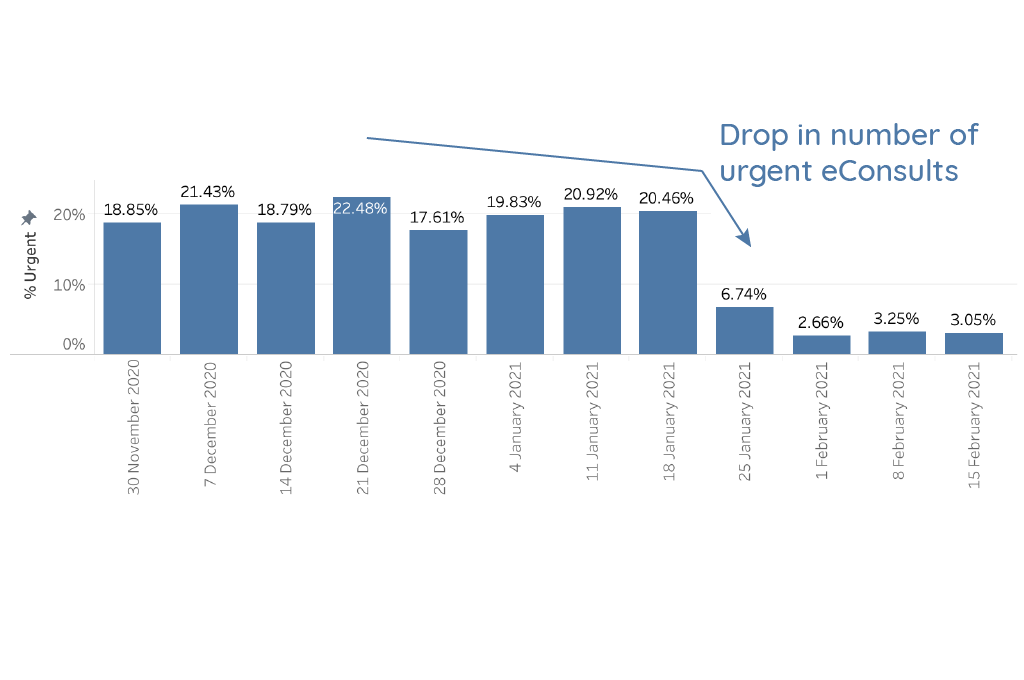
The follow-up data is very promising, with a substantial reduction in ‘urgent’ eConsults across the MSK questionnaires we’ve adjusted (see graphs below – changes made around the 25th January 2021). Across these questionnaires, on average 9% are now marked as urgent, instead of the 17% that existed before the changes.
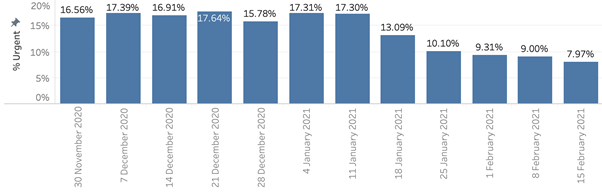
As examples across specific questionnaires, the percentage of urgent Foot Pain eConsults dropped from around 16% to around 9%, with similar reductions seen in Back Pain and even greater reductions seen in Shoulder Pain (from around 20% to around 5% after implementing the functional pain scores). We are continuing to monitor this to see if further improvements can be made.
What next?
Improving the pain scoring across the MSK questionnaires is just the start. We knew that these questionnaires in particular were causing some patients to be directed to more urgent care unnecessarily. We can now start to look at other areas to test and potentially update. Watch this space!
eConsult is fundamentally built on ensuring patient safety. We include multiple levels of clinical safety net so that no patient comes to harm while using eConsult. As more patients continue to use online consultation platforms, this level of safety is essential for any provider. As a company, we are working hard to improve the user experience, while maintaining patient safety. We constantly monitor and tweak our content to ensure we get the right balance.
Get in touch if you would like a demo of any of eConsult’s features
Written by:
Dr Aravinth Balachandran, MRCGP, BSs | Chief Medical Officer.
Aravinth qualified from the University College London Medical School in 2002 and has been working as a qualified GP since 2008. A Partner at his practice, Aravinth currently sees patients at Oaklands Health Centre in Hythe, Kent.